Diabetes Information
What is Diabetes
What is Diabetes?
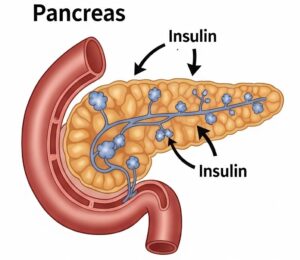
Diabetes is a long term health condition that happens when your body can’t make enough insulin or doesn’t use it the right way. Insulin is a hormone that helps move sugar (glucose) from your blood into your cells to give you energy. Insulin is produced by the beta cells in the pancreas. Insulin helps cells absorb glucose (sugar) from the bloodstream, using it for energy or storing it for later. When blood sugar levels rise, the pancreas releases insulin to help bring them back down.
When insulin doesn’t work well or isn’t there, too much sugar stays in your blood. This leads to high blood sugar levels, which can be harmful over time.
Why It Matters:
If diabetes isn’t managed, it can cause serious problems like heart disease, kidney damage, nerve pain, and vision loss. The good news is that with the right care, people with diabetes can live long, healthy lives.
TYPES OF DIABETES
Type 1 diabetes is an autoimmune condition where the body’s immune system attacks and destroys the insulin producing beta cells in the pancreas. As a result, the body produces little or no insulin, a hormone necessary for regulating blood sugar levels. While the exact cause is not fully understood, a combination of genetic factors and environmental triggers, such as certain viral infections, are believed to play a role. Unlike Type 2 diabetes, it is not related to lifestyle or diet.
Symptoms: Type 1 diabetes is usually diagnosed in children, teenagers, or young adults, although it can occur at any age. Common symptoms include frequent urination, extreme thirst, unexplained weight loss, fatigue, irritability, blurred vision, and in some cases, fruity smelling breath, which can signal diabetic ketoacidosis (a serious complication). Since the body cannot produce insulin, people with
Treatment: Type 1 diabetes need daily insulin therapy through injections or an insulin pump. Managing this condition also involves regular blood sugar monitoring or the use of continuous glucose monitors (CGMs), a healthy diet, and exercise. If not properly managed, Type 1 diabetes can lead to complications such as heart disease, kidney problems, nerve damage, and eye issues.
Type 2 diabetes is a metabolic disorder in which the body either doesn’t use insulin effectively (insulin resistance) or doesn’t produce enough insulin to maintain normal blood sugar levels. Initially, the pancreas may compensate by producing more insulin to maintain normal blood sugar levels, but over time, its capacity is overwhelmed, leading to persistent hyperglycemia. This type is much more common and is strongly linked to lifestyle factors, including poor diet, physical inactivity, and being overweight or obese. Genetics also play a role, and certain ethnic groups such as African American, Hispanic, Native American, and South Asian populations are at higher risk.
Prediabetes: This is an intermediate condition where blood sugar levels are higher than normal but not yet high enough to be classified as full blown diabetes. Prediabetes is particularly noteworthy because it is considered a potentially reversible condition, offering a critical window for intervention to prevent progression to Type 2 Diabetes.
Symptoms: Though it traditionally affects older adults, Type 2 diabetes is increasingly being diagnosed in younger people, including children. Symptoms of Type 2 diabetes often develop slowly and can include increased thirst and hunger, frequent urination, fatigue, blurred vision, slow healing wounds, and numbness or tingling in the hands or feet. Many people may not realize they have it until complications arise.
Treatment: Treatment typically starts with lifestyle changes like adopting a healthier diet, exercising regularly, and losing weight. Oral medications such as metformin are commonly used, and insulin therapy may become necessary as the disease progresses. With proper management, people with Type 2 diabetes can prevent or delay complications, but if left uncontrolled, it can lead to serious issues such as heart disease, kidney failure, nerve damage, and vision loss.
Gestational Diabetes: This form of diabetes is diagnosed during the second or third trimester of pregnancy in women not previously known to have diabetes. It arises from an inadequate pancreatic beta cell response to the significant insulin resistance induced by pregnancy hormones. Hormones produced by the placenta, such as estrogen, cortisol, and human placental lactogen, create a “contra-insulin effect,” rendering the body’s insulin less effective, typically starting around 20 to 24 weeks of gestation. While the pancreas normally increases insulin production to compensate, gestational diabetes occurs when this compensatory mechanism is insufficient. A defining characteristic is that symptoms usually resolve after delivery.
Can Diabetes be reversed?
The concept of “diabetes reversal” primarily applies to Type 2 Diabetes and Prediabetes, where significant evidence supports the possibility of achieving normoglycemia without medication. For Type 1 Diabetes, the term “reversal” is not used in the same context due to its autoimmune nature and absolute insulin deficiency; instead, research focuses on functional restoration through advanced therapies. Click on the link below for a detailed analysis of diabetes reversal:
Table: Comparing Major Diabetes Types
| Feature | Type 1 Diabetes | Type 2 Diabetes | Gestational Diabetes |
| Primary Root Cause | Autoimmune destruction of pancreatic beta cells | Insulin resistance and progressive beta cell dysfunction | Pregnancy-induced insulin resistance and inadequate beta cell response |
| Key Pathophysiological Mechanisms | T cell mediated insulitis, autoantibody production, absolute insulin deficiency | Impaired insulin signaling in target tissues (muscle, fat, liver), inflammation, oxidative stress, lipotoxicity, beta cell failure | Placental hormone-induced “contra-insulin effect,” reduced incretin secretion, beta cell dysfunction |
| Role of Insulin Resistance | Can develop, but not primary cause | Central and primary defect | Primary driver, induced by pregnancy hormones |
| Role of Beta Cell Dysfunction | Absolute deficiency due to destruction | Progressive loss of adequate insulin secretion | Inadequate response to increased insulin demand |
| Typical Onset Characteristics | Often sudden, severe symptoms; usually childhood/adolescence, but can be any age | Gradual, often asymptomatic; typically adulthood, but increasing in children | During pregnancy (2nd/3rd trimester); usually asymptomatic |
| Potential for Reversibility | Not currently reversible (focus on functional normalization via cell replacement/immunomodulation) | Potentially reversible, especially with significant weight loss and early intervention | Usually resolves post delivery, but increases risk of future Type 2 Diabetes |
01.
Symptoms
Here are the most common symptoms of diabetes, especially in Type 1 and Type 2 diabetes. These symptoms occur due to high levels of glucose in the blood and insufficient or ineffective insulin.
1. Frequent urination – The kidneys work overtime to filter and remove excess sugar through urine.
2. Excessive thirst – Caused by dehydration from frequent urination.
3. Unexplained weight loss – The body starts breaking down muscle and fat for energy when it can’t use glucose.
4. Increased hunger – Glucose isn’t reaching cells, so your body signals for more food.
5. Fatigue – Lack of insulin or insulin resistance prevents sugar from entering cells for energy.
6. Blurred vision – High blood sugar causes swelling in the lens of the eye.
7. Slow healing wounds or frequent infections – High blood sugar impairs the immune system and blood flow.
8. Numbness or tingling in hands and feet – A sign of nerve damage (diabetic neuropathy) from prolonged high blood sugar.
9. Other Possible Signs – Dry skin or frequent skin infections; Irritability or mood swings; Dark patches of skin, especially around the neck or armpits.

02.
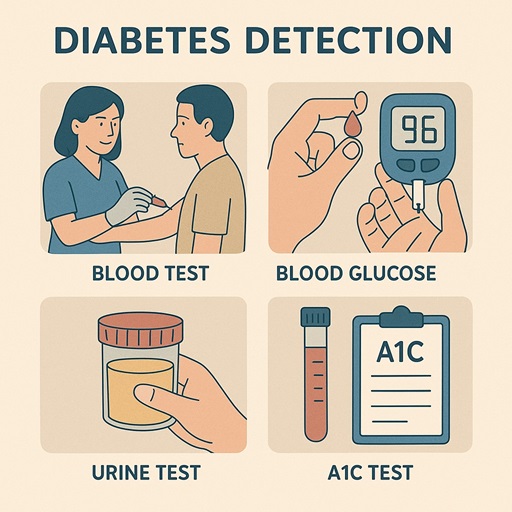
Detect
Detecting diabetes involves medical tests that measure blood sugar (glucose) levels. These can identify whether you have diabetes, prediabetes, or normal blood sugar levels.
1. Fasting Blood Sugar (FBS) Test
What it is: Measures blood glucose after not eating for at least 8 hours.
Normal: Less than 100 mg/dL
Prediabetes: 100–125 mg/dL
Diabetes: 126 mg/dL or higher on two separate tests
2. HbA1c (A1C) Test
What it is: Measures your average blood sugar over the past 2–3 months.
Normal: Below 5.7%
Prediabetes: 5.7%–6.4%
Diabetes: 6.5% or higher
3. Oral Glucose Tolerance Test (OGTT)
What it is: Measures how your body handles sugar before and 2 hours after drinking a sugary drink.
Normal (2 hr): Below 140 mg/dL
Prediabetes: 140–199 mg/dL
Diabetes: 200 mg/dL or higher
03.
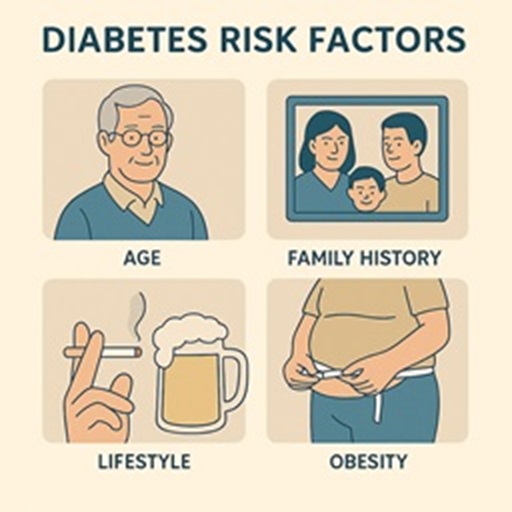
Risk Factors
The cause of diabetes depends on the type. In all cases, the underlying problem is related to how your body processes glucose (sugar) and uses insulin.
1. Type 1 Diabetes – Autoimmune Reaction
Cause: The immune system mistakenly attacks and destroys the insulin producing beta cells in the pancreas.
Result: The body produces little or no insulin.
Trigger factors:
Genetic predisposition
Environmental triggers (possibly viruses, diet, or stress in early life)
2. Type 2 Diabetes – Insulin Resistance
Cause: The body’s cells become resistant to insulin, and the pancreas can’t make enough to keep blood sugar normal.
Root contributors:
Obesity, especially belly fat
Lack of physical activity
Poor diet (high sugar, high refined carbs)
Genetics (family history)
Aging – risk increases with age
Chronic stress & poor sleep
Inflammation & hormonal imbalances
3. Gestational Diabetes – Hormonal Effects in Pregnancy
Cause: Hormones from the placenta block the action of the mother’s insulin (a natural form of insulin resistance).
Risk factors:
Overweight before pregnancy
Family history of diabetes
Ethnic background
Previous large baby or gestational diabetes
04.
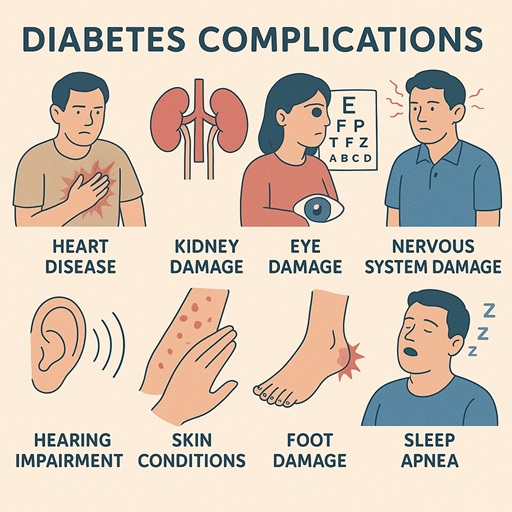
Complications
Diabetes, when not well controlled, can lead to serious short term and long term complications affecting nearly every organ system in the body. These complications arise primarily due to prolonged high blood sugar (hyperglycemia), which damages blood vessels and nerves.
1. Brain & Nervous System
Stroke – Due to damage in brain blood vessels
Neuropathy (nerve damage) – Especially in legs and feet, causing:
Numbness, tingling, burning pain
Loss of sensation → higher risk of injuries and infections
2. Eyes
Diabetic retinopathy – Damage to retina, can lead to blindness
Cataracts – Clouding of the eye lens
Glaucoma – Increased eye pressure damaging the optic nerve
3. Heart & Blood Vessels
Heart disease (coronary artery disease)
High blood pressure
Atherosclerosis (narrowed arteries)
Increased risk of heart attack and stroke
4. Limbs (Especially Feet)
Foot ulcers – Due to poor circulation and nerve damage
Infections – Can become severe or chronic
Amputation – In extreme cases due to gangrene or untreatable infections
5. Kidneys
Diabetic nephropathy – Damage to kidney filters
Can lead to chronic kidney disease or kidney failure (dialysis may be needed)
6. Metabolic & General
Diabetic ketoacidosis (DKA) – Life threatening, mostly in Type 1; body breaks down fat too fast
Hyperosmolar hyperglycemic state (HHS) – Mainly in Type 2; severe dehydration and very high blood sugar
Frequent infections – Skin, gum, urinary tract
Delayed healing – Especially for cuts or wounds
7. Cognitive & Mental Health
Increased risk of dementia and Alzheimer’s
Depression and anxiety – Common in people with long term diabetes