Diabetes Reversal
Can Diabetes be reversed?
Insulin Resistance
Lifestyle Change
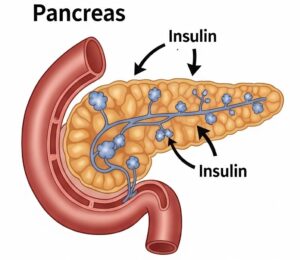
Beta Cells
Sustainable Health
Diabetes Reversal Research
Is diabetes reversal feasible?
Growing research confirms that type 2 diabetes is not necessarily a lifelong, progressive condition. Several clinical studies show that with targeted lifestyle interventions (particularly diet, exercise and structured coaching), many individuals can achieve diabetes remission or even reversal.
1. DIADEM-1 Trial (Weill Cornell Medicine, Qatar)
- A 1-year intensive lifestyle program combining a low-calorie diet and exercise led to an average weight loss of ~12 kg.
- 61% of participants achieved diabetes remission, compared to 12% in standard care.
- Over 30% regained normal blood glucose levels.
- Reference: The Lancet Diabetes & Endocrinology (2020)
- Summary: Weill Cornell Medicine Newsroom
2. DiRECT Trial (United Kingdom)
- A structured very low-calorie diet (~825–853 kcal/day) for 3–5 months followed by food reintroduction produced remarkable outcomes.
- 46% of participants were in remission after 12 months, versus 4% in usual care.
- Reference: The Lancet (2017)
- Summary: NIHR Evidence
3. University of Michigan Study
- Participants following very low-calorie or ketogenic diets achieved 47% remission at one year and 38% maintained remission at two years.
- These approaches also dramatically reduced the need for insulin and other medications.
- Summary: University of Michigan News
4. Virta Health Program (Remote Care + Nutritional Ketosis)
- In a two-year digital health program focused on nutritional ketosis and remote coaching:
- 38% achieved diabetes reversal, and 55% of active participants maintained sub-diabetic HbA1c without medications.
A five-year follow-up confirmed 20% in remission and 32.5% maintaining reversal with sustained improvements in cardiovascular and metabolic health. - Reference: Diabetes Research and Clinical Practice (2024)
- Summary: virtahealth.com
5. Precision Nutrition and Exercise Program
- A one-year personalized diet and exercise plan lowered average HbA1c from 8.9% to 6.1%, with 78% of participants achieving diabetes reversal.
- Source: Endocrine Practice Journal
6. UCLA Intensive Short-Term Program
- Even brief interventions can make a difference.
A 3-week high-fiber, low-fat diet plus 45–60 minutes of daily exercise led to reversal of type 2 diabetes or metabolic syndrome in 50% of participants, even without major weight loss. - Summary: ScienceDaily
Conclusion
- Lifestyle transformation works: Sustained dietary change, weight reduction, and physical activity are central to diabetes reversal.
- Earlier intervention = higher success: The shorter the duration since diagnosis, the greater the chance of remission.
- Structured support matters: Programs with coaching and follow-up yield better long-term results.
- Reversal ≠ cure: Ongoing lifestyle maintenance is crucial to prevent relapse.

